First of all, this is work outside a medical institution: a street, an enterprise, a public transport salon. At best, an apartment. The possibilities of the doctor are limited, he is constantly in the "zone of action" of three deficits: time, money, information. These factors create a certain tension.
Another one distinguishing feature- Lack of a permanent job. An ambulance doctor (paramedic) is always surrounded by people who are unfamiliar with his work: relatives of the patient, his employees, or just passers-by on the street. The absence of a permanent workplace leaves an imprint on the psychological attitude of the doctor and the team as a whole. There is nothing of this in the work of a doctor in a hospital or even a polyclinic, where the doctor works among colleagues and he has a permanent workplace, where no one interferes, does not make comments, does not give advice (when it is not asked for). In extreme conditions, when the nerves are more or less tense, there are more conditions for making a mistake (diagnostic, tactical, deontological), especially if there is no experience, professional training that could help in such situations. Of course, an extreme situation cannot justify the doctor's sins, but it certainly should be taken into account when analyzing the reasons. All of the above factors, especially when working with antisocial patients, or deaths in the presence of a doctor, especially during transportation, when, being in a confined space, he has exhausted his ability to save the patient - do not pass without a trace for his nervous system, psyche. In the scientific literature in recent years, there have been works devoted to this problem, which is called " emotional burnout or "emotional burnout". At some stations (Chelyabinsk, Perm, Tyumen) there is a medical and psychological service, the task of which is to minimize the negative effects of this syndrome, to relieve stress, especially among recently arrived workers. The expected result is the preservation of the health of the personnel, the reduction of staff turnover, which today is the primary task of the leaders of the ambulance service. In one of these works, the authors emphasize that “professional activity that constantly takes place in extreme conditions and in emergency situations leads to a decrease in the level of professional health, reduces the quality professional activity and worsens the psychological climate in the team.
However, the doctor should not be lost in critical situations. It is to the work of an ambulance that the phrase that “delay is similar to death” applies. On the tomb of the Roman emperor Hadrian, the words are inscribed: "The confusion of the doctor is disastrous for the patient."
“Treatment should be timely, as early as possible and as soon as possible”,- these words refer to all levels of health care, but first of all - to the ambulance, they belong to Professor L. A. Leshchinsky, whom we have already mentioned, who is a recognized authority in our service.
In recent years, due to the stagnation of the polyclinic link, the number of chronic patients who do not receive proper treatment has become much larger, which has led to an increase in the burden on the ambulance. But such patients are not only at home, they often come to the clinic, which is far away. not always ready to provide emergency assistance
Here is one example:
An ambulance station received a call to one of the city's clinics about the onset of clinical death in a patient who came to the reception. The doctor of the cardiological team, who arrived after 26 minutes (taking into account the lack of teams and our today's traffic jams, is a good result), was given the duty phrase: "While you wait, you can die, the patient has already died." The patient was in the office of the head of the clinic. What kind of help was provided to the patient while waiting for the brigade? The reader has already guessed - no! Disagreeing with the diagnosis, without wasting time on discussions and on " воспитание!}» polyclinic staff, doctor O. V. Sitnikova carried out the necessary set of resuscitation measures. As a result of the competent actions of the entire team, the patient was brought out of the state of clinical death and hospitalized in the Clinical Diagnostic Center "Cardiology". Diagnosis, -a; m. A brief medical report on the disease and the patient's condition, made on the basis of an anamnesis and a comprehensive examination. From Greek. — recognition, diagnostics, and; and. 1. A set of techniques and methods, including instrumental and laboratory ones, that allow to recognize the disease and establish a diagnosis. From Greek. - able to recognize. 2. Diagnosis, dialysis, -a; m. peritoneal dialysis. A method for correcting water-electrolyte and acid-base balance and removing toxic substances from the body with the introduction of a dialyzing solution into the abdominal cavity.
" data-tipmaxwidth="500" data-tiptheme="tipthemeflatdarklight" data-tipdelayclose="1000" data-tipeventout="mouseout" data-tipmouseleave="false" class="jqeasytooltip jqeasytooltip19" id="jqeasytooltip19" title=" (!LANG:Diagnosis">Диагноз!}, myocardial infarction was confirmed clinically.And here is another case.
01/24/08. cardiological team of the ambulance station consisting of: doctor Zubritskaya, paramedic O. Chikantseva. driver V. Leskin went to one of the city clinics. When collecting an anamnesis, the doctor found out that the patient had come to see the surgeon about a wound on the stump of leg e (he wears a prosthesis). Entering the clinic, he suddenly felt intense pain behind the sternum. It was filmed, on which signs of ischemia were recorded along the anterior and lateral walls of the left ventricle. In the clinic, the patient was administered: Ketorol - 30 mg, Cordiamin 2.0, Sulfocamphocaine 2.0 (the route of administration was not specified). The author specifically lists the administered drugs in order to demonstrate the "adequacy" of anesthesia for a coronary patient in the 21st century! The cardiology team was called for hospitalization. From the entry in the card of the doctor M. Zubritskaya: “He lies on a bench, in the hall near the reception. Nearby - a medical registrar and a security guard (!). Complaints: intense pain behind the sternum, their duration is more than 30 minutes.
Author's note: The ECG room is located on the second floor, the reception, near which the patient was lying, is on the first floor. This means that after recording the ECG, which had the symptoms described above, the patient, and even without one leg, (not anesthetized!) Was allowed to go down on foot to the first floor.
We read the call card further: “The patient was anesthetized. During his loading into the ambulance, a state of clinical death suddenly developed. Resuscitation measures were immediately started: indirect heart massage, mechanical ventilation with an AMBU bag, EITD with a discharge of 250 J. Within 1 minute, consciousness and spontaneous breathing were restored. BP - 130/80 mm Hg, heart rate - 100 in 1 min. The patient was taken to the Clinical Diagnostic Center "Cardiology". (For ethical reasons, we do not name the place of action, we will only say that both of these cases took place ... in the same clinic).
As of 06.02.08. - the patient from the intensive care unit was transferred to the ward. It is quite logical to assume that a gross violation of the regime: a patient with acute myocardial infarction (not anesthetized), was allowed to go down from the second floor - and could be the cause of clinical death. Only thanks to the competent actions of the medical team of M.F. Zubritskaya, the patient survived.
Ambulance- a good school for a doctor. The experience gained in the ambulance turns out to be useful, even if later the doctor chooses another specialty (the dean of the medical and preventive faculty of the Ural State Medical Academy, Professor A. N. Andreev, rightly believes that it cannot be a good doctor, in particular, family, one that did not work in an ambulance. It is not difficult to guess what is behind these words - personal experience Arkady Nikolaevich). The head of the department of toxicology and emergency medical care of our academy, Professor V. G. Sentsov, also recalls with gratitude the years of work at the station. Probably, we will not give away secrets if we say that the head of the Health Department of our city, A. I. Prudkov, also worked at an ambulance station in the Kirovsky district. Therefore, one should welcome and strongly encourage those students who, even before graduation, go to work for an ambulance. It is no coincidence that they say that a student working at an ambulance station is a potential emergency doctor. These are the most valuable shots. The only pity is that our legislators do not understand (or do not want to understand) this truth. In historical materials on ambulance, draws внимание!} the fact that at all times medical students have taken an active part in the work of this important rescue service. We periodically conduct a survey of students who have completed the SMP cycle. Briefly summarizing the statements of the respondents, we can say that they all believe that the cycle is necessary, and, moreover, regardless of the specialty chosen by the graduate. Students also like the fact that the doctor immediately sees the results of his work. They also note the benevolent attitude of almost all substation workers towards students, and some who have shown special diligence are invited to come to work.
The names of many doctors who hold fairly high positions are known, who combined their studies with work in an ambulance or worked in an ambulance after graduating from a university. None of them speaks of these years as if they were lost. They remember their work at the ambulance station with gratitude. In addition to those mentioned above, we will name one more name. N. A. Lengauer began her journey at the ambulance station in Kyiv as a nurse. Many years later, the ambulance station headed by Natalya Andreevna, according to colleagues from other cities of the Union, was considered the best. The station was honored to be the WHO base for training cadets for ambulances, and the chief doctor received the title of Hero of Socialist Labor.
IS IT POSSIBLE TO BE OFFENDED AT THE SICK?
IN AND. Belokrinitsky, Yekaterinburg
Interesting question, isn't it? Formally - it is possible, and at first glance - it is possible: He is the same person ...
Once upon a time, the radio play “Doctor Zhukov, on call” was often broadcast on the radio, this is about the work of a regional emergency station in Moscow. In this performance, R. Plyatt played the role of Dr. Zhukov with his characteristic brilliance. According to the play, this is a doctor wise over the years and experience, from whom it is not a sin to learn from young people. So he said: “We sometimes take offense at the sick, because we misunderstand the word“ sick ”. Sick is not a noun, sick is an adjective for the word "person". Sick person. And a sick person, due to his illness, has an altered psyche, he is exhausted by prolonged pains, and perhaps by repeated, and even ineffectual walking on medical offices. The ambulance doctor is in a special position. Sometimes an ambulance is called, not having received a referral to the hospital from “their”, district doctor, or not waiting today for a doctor from the clinic, but you never know what else! Even a conversation with the dispatcher prior to the arrival of the brigade can lead to sick person"out of myself". And all the accumulated negative will be splashed out on the one who is most available, and from whom you can get the most specific and real help. Well, isn't it a paradox? Sometimes, as soon as the doctor crosses the threshold of the apartment, a stream of claims immediately falls upon him, which are directed at the wrong address. Why is he (she) not admitted to the hospital, why are there no necessary medicines, etc. The emergency doctor is mistaken for at least the medical inspector of the district health department! By the way, this indicates the level of education of the population, because many do not even understand that a polyclinic and an ambulance are completely different institutions with completely different tasks, which makes it pointless to make claims to the ambulance doctor in the work of the polyclinic. I repeat, the emergency doctor is the most accessible. After all, it is not for nothing that ambulances are called the frontier of healthcare. Here is the "forefront" and gets it!
But here you are “attacked” with a stream of claims to which you have nothing to do. Start immediately "defend" when the patient (or relatives) are still hot? This energy will involuntarily be transferred to you (mirror effect), you will get involved in a conflict, and it is possible that you will suffer from it. How to be? There is such an approach. Ask the essence of the claim (knowing very well that it is not for you) to state it again, explaining that you did not understand something. (Just don’t interrupt the patient, let him speak. The time spent on this will pay off by preventing a conflict, maybe even a complaint, which will then take much more time to resolve and not one, but several people. Do not forget to reflect this situation in the call card).
You will notice that there will be less emotions. In extreme cases, you can ask to repeat some part of the entire claim again. The conversation will be very calm. You have given the patient the opportunity to "let off steam." This is just one way to avoid conflict. The task of the doctor is to prevent its development. There is a folk wisdom: "Of the two arguing, the one who is smarter is to blame". And since you naturally consider yourself smarter, so try to make sure that the fire does not flare up. Firefighters have a good term: "Localize the fire." It should be clear to the doctor, as a firefighter, that after the focus is localized, it is easier to extinguish it.
Try to keep the members of your brigade from taking part in this duel. It will be easier for you. Here is the answer to the question: “Is it possible to be offended by a sick person?” Forgive him! He's sick. Leave your ambitions for later. After all, we are doctors, we serve the profession, and do not “sell a service”, as we often hear about this, especially lately.
True, sometimes one has to come across facts of obvious “courage” over medical workers on the part of patients and not so much seriously ill, but those who are not so much sick as they want to “shake their rights”: “you were called, you must”, etc. I'm not going to justify them, of course, this is a manifestation of low culture. More precisely - lack of culture. Perhaps one of the reasons is the costs of the ideology of the previous government: free medicine, and free medicine was identified with “costs nothing”. And what is worth nothing is not appreciated. This is the result of a fundamentally erroneous thesis of the same ideology that attributed medicine to the service sector. But even A.F. Bilibin said that medicine is a service, not a service.
On this occasion, our colleague, an ambulance doctor, once said that “ if medicine is classified as a service sector, then saving a patient from pulmonary edema or selling a kilogram of sugar is one and the same. You better not say! Indeed, how far one must be from emergency medicine, what is medicine - ordinary human morality, to call, say, bringing out of clinical death - a medical service! I do not justify such "ideologists". Just when you understand “Pathogenesis, [ne]-a; m. The mechanism and sequence of the appearance and development of the entire cycle of a disease process or disease as a whole, starting from its beginning. From Greek. pathos—suffering, disease, and... genesis.
" data-tipmaxwidth="500" data-tiptheme="tipthemeflatdarklight" data-tipdelayclose="1000" data-tipeventout="mouseout" data-tipmouseleave="false" class="jqeasytooltip jqeasytooltip16" id="jqeasytooltip16" title=" (!LANG:Pathogeny">патогенез », легче понять мотив, побудивший к такому поведению. А, уяснив - никогда не опускайтесь до взаимных оскорблений, выражения обиды. Это не тот случай. Будьте выше этого, неважно, врач вы или фельдшер. Нужно уважать себя, тогда и другие будут вас уважать. И вот случай, который недавно имел место.!}17.12.06. At 1:57 a.m., a call was received to the dormitory of the law academy. The reason is trauma. After 16 minutes, the brigade arrived at the scene. Upon arrival, it turned out that the "victim" - a fourth-year student of the academy (almost a graduate!) in a state of intoxication, "threatened to beat others, knocked on the walls, doors with his fist, pounced on the guards," - verbatim is the entry from the call card. However, the doctor tried to examine the "patient" to make sure that help was needed. We read further: "During the inspection - threatens." This whole story had a logical conclusion - "sick" i.e. the drunken brawler was handed over to the police.
As a result, 55 minutes were spent on the call. The average cost of calling a line crew is within 1,500 rubles. Who should pay for this challenge? Or maybe at this time someone really needed emergency assistance, and the brigade was busy, now you already know where.
We live in a time when the doctor is practically not protected by anything, as a rule, the judiciary comes to the defense of the opposite side, sometimes at the suggestion of the media. This is explained to us by the peculiarities of the market economy. But then let's continue the comparison, and if higher demands are made on medicine, then it's time to solve the long-term problem of responsibility for disrespect for a doctor (paramedic), for an unreasonable (false) call, as is the case, for example, in the USA. And this is also deontology, since, demanding a proper attitude on the one hand, the same requirements must be made on the other. Otherwise, this is not mutual respect, but servility. You can not play with one goal!
And as if to confirm the correctness of this thought, I would like to quote a fragment of the resolution of the II All-Russian Congress of Emergency Physicians, which was held in Moscow on October 31 - November 2, 2007:
3. Consider it strategically important and significant for the country and the healthcare system itself to immediately begin to complete the formation of the legal framework for effective work emergency medical care, taking into account the requirements of the socio-economic transformations that have taken place in the country and in this regard. on behalf of the entire medical community, to urge the State Duma of the Federal Assembly of the Russian Federation to prepare and submit for discussion draft laws:
... « About the rights and responsibility(highlighted by the author) patients in Russian Federation».
It gives hope for success that the new generation of leaders holds the same point of view. In an interview with the Moscow newspaper "Medical Vestnik" (03/28/08), the newly appointed Minister of Health Sverdlovsk region, V. G. Klimin reasonably stated that “We need to care not only about the rights of the patient, but also about the rights of physicians.”
By the way, you will not see anything like this abroad, “among the damned capitalists”, with whom the “native communist government” has been scaring us all the time. There, medicine is one of the respected (perhaps because of the highly paid) specialties. A call to the sick (injured) pays Insurance Company. And this despite the fact that the doctor does not go to the patient.
(When the first demonstration of the American series Ambulance ended, at a meeting with Moscow ambulance workers, TV presenter Arina Sharapova asked our Moscow colleague, what is the difference between our ambulance and the American ambulance? And he replied: “We have a doctor going to the patient, they have the patient is being taken to the doctor. But if the call is unreasonable - the caller pays a fine, and the amounts are quite impressive!
.
Target: Introduce the concept of professional communication. To give a general idea and highlight the features of the psychology of communication between a medical worker and patients. Introduce the concepts of "asthenization" and "neuroticization". Offer a detailed plan for the conversation of a medical worker with a patient in an inpatient treatment setting.
Prepare students to master the following professional competencies: PC 1.1; PC 2.3; PC 2.5; PC 2.6; PC 2.7; PC 3.2; PC 3.3; PC 3.4; PC 3.6.
Professional communication , being one of the options for interpersonal communication, is determined by the type of profession, the goals and objectives of a particular professional activity, its social significance. Each professional activity is based on the knowledge and skills necessary for its implementation, has its own linguistic, ethical, material and technical base, features of organization and management. Depending on the type of professional activity in the minds of people, certain representation about the image of the bearer of a particular profession. So, for example, an artist must be beautiful and sensual, an athlete must be strong, an astronaut must be well prepared and fearless.
- Do you remember what this phenomenon is called in psychology?
This is the phenomenon of stereotyping, stereotypical perception.
- What is the image of a medical worker in the minds of people?
The medical worker should, in the opinion of society, have an education, deep knowledge in their specialty, be a highly moral person. Moreover, it must have personal charm, modesty, truthfulness, justice, humanism and remain throughout life a healthy person . At the same time, medical activity is carried out within a number of legal administrative normative boundaries that can influence the nature of professional activity. These are strict subordination, normative loads, mandatory execution, examination procedure, etc.
Orientation of professional communication dual. First turn this is intraprofessional communication. Interprofessional medical communication is based on the necessary knowledge of medicine and its language. The first ones are constantly replenished, and the language is based on a large amount of Latin terminology, which is practically not used in everyday life. Medicine has a huge number of sections and specialties, each of which has its own specifics. In solving the problems of protecting human health, medicine is structurally organized in a certain way and is implemented at different executive levels (institution, department; doctor, paramedic, nurse, orderly). Besides, medical activity , despite the importance of the central figure of the doctor, is a collective activity.
The focus on Latin, as the basic language in medicine, has historically pursued the goal of creating the possibility of mutual understanding between medical workers, regardless of their national language. In addition, it made it possible to restrict access to content medical reports outsiders. At present, its importance in maintaining medical secrecy has somewhat decreased, but it still plays an intraprofessional communicative role. Therefore, the more knowledge of medical terminology a medical worker has, the easier it is for him to understand his colleagues, regardless of their specialization.
The organization of medical activities is aimed at the maximum limitation and exclusion of actions that can harm the patient.
- What is the main principle of the work of a health worker? ("Do no harm!")
This obliges the health worker to observe strict subordination in communication and work. The personal initiative of the health worker should not go beyond the actions provided for by a specific plan for the examination and management of the patient.
The collective nature of medical activity also implies the need to form a sense of collectivism, mutual respect, mutual trust and mutual responsibility among employees.
- Remember the work of the ambulance crew from the movie "Ambulance".
Secondly professional communication of a health worker includes communication with patients.
With the improvement of the diagnostic and treatment process, the introduction modern methods treatment and diagnosis, inevitably increasing demands on the paramedic , to his personal and professional qualities. The patient sees in the medical worker a representative of the profession, a specific specialist, just a person, finally. Consciously or unconsciously, the patient evaluates the health worker. To address such questions: “Can this specialist be trusted?”, “What kind of person is he?” Depending on what opinion is formed by a person who turned to you for help or was forced to receive it from you, the effectiveness of your help will be largely determined.
- We have already said that a certain image of a medical worker is being formed in society.
The more the patient matches the expected image of a medical worker with a real, greater trust he feels for him. It is no coincidence that specialists in medical psychology believe that a medical worker should impress good man". It is to such a person that the patient will want to entrust his health and life. It is on this complete trust of the health worker and the patient that therapeutic cooperation is built, without which treatment is impossible.
Currently, the need for an individual approach to the patient is increasing. In this regard, the paramedic requires not only high professionalism, but also knowledge of the psychology of communication, deep assimilation of ethical norms and rules of deontology.
- Even Avicenna, the great physician and thinker of the Middle Ages, spoke about three means of helping a sick person - about "a knife, grass and a word", thereby emphasizing the importance of a human word, and in fact - the psychology of communication in the process of healing from an illness.
When communicating with a patient, the health worker should be aware that any disease is strong enough stress-causing factor . This inevitably affects the mental well-being of the patient, even if it is not realized by him. The tension of various functional systems of the body contributes to the overall asthenia(weakening and exhaustion of adaptive mechanisms and, first of all, the central nervous system) and neuroticism(appearance of various pathological personal reactions). This is especially evident in long-term chronic diseases. All this complicates the process of communication and interaction with the patient.
- What do you think is the most difficult thing in the work of a paramedic?
The most difficult thing in the work of a paramedic is the process of communicating with a sick person; communication, which is significantly different from communication with a healthy person.
The health worker must be able to timely assess the neuropsychic state of the patient and, if possible, have a beneficial effect on the patient in the process of communication. He must be able to assess the impact on the patient's psyche of the characteristics of the course of the disease, diagnostic procedures, the effect of the treatment. In this case, the main symptom of assessing the patient's condition will be pain, and its successful overcoming will be the main factor in providing assistance.
Other factors will also indicate the deterioration of the patient's condition. For example, if the patient withdraws into himself, becomes lethargic, indifferent. Quite often, the deterioration of the condition manifests itself in the form of anxiety, irritability and even aggressiveness. All this medical worker should notice in time, understand and adequately evaluate. About all cases of changes in the state of health and the patient's condition, the medical worker must inform the doctor in time.
In the fight against the disease, much depends on the patient, on his resilience, willingness to cooperate with doctors. The health worker must be able to to help the patient realize the need to fight the disease. (Abul Faraja, XIII century).
In this regard, an important psychological task of the paramedic is the ability to involve the patient in active participation in the treatment process.
2. Communication with patients.
What are the patterns in establishing contact and interaction between a health worker and a patient?
Ishwan Hardy singled out three stages in the communication of a health worker with a patient in the conditions of inpatient treatment:
At the first, initial stage orientation takes place: the patient and the health worker get to know each other. And although a sick person is immersed in his problems, but in the interests of adapting to a new situation, he is forced to make contact with the people around him, take into account the specifics of the hospital environment, and reckon with accepted rules. In turn, the paramedic or nurse, during the acquaintance, gets an idea about the behavior of a new person, his character traits, feelings, goals, which is very important in future work. The patient during this period may be overcome by memories of a previous stay in the hospital, prejudices that he can project onto the attending staff.
At the second extended stage , the patient and the medical staff, having met, build their communication with each other depending on the existing level of relations. At this stage, the patient's condition largely depends on the changes that occur to him as a result of the disease. This is how fear, uncertainty, morbid fantasies, suspiciousness, pickiness, etc. appear. Support for the patient, positive changes in the state of health, trusting relationships with medical personnel, a constructive climate in the department - all these are the factors that bring a sense of optimism into the patient's consciousness, hope for a favorable outcome, recovery.
At the final stage Difficulties arise when the patient is discharged. He has to leave a place where he is protected from danger, and this causes anxiety. The state of uncertainty is exacerbated by concerns about whether he will be able to fully engage in everyday life and work. At this stage, it is important to prepare the patient in advance for discharge, to help him comprehend the options for subsequent actions. The tasks of the doctor and medical staff are also in the psychological preparation of relatives and friends of the patient on how to support the discharged person, what to do in this or that situation at home.
Important in communicating with patients during treatment is creation rack feedback . In parallel with the treating specialist, the patient monitors his condition and, as necessary, analyzes his findings together with specialists. When working in tandem with a doctor, a medical worker is obliged to agree with him on the amount of information that she can bring to the attention of the patient and his relatives. Wherein it does not follow inform in a hurry, “on the go”, or in front of outsiders. Rudely or abruptly interrupt the patient's emotional reactions. It is forbidden give explanations that are obviously incomprehensible to the patient and “frighten” him. It is forbidden make promises that cannot be kept or withhold information in order to "reassure". It does not follow to be ironic about the disease, to interpret the actions of the medical staff negatively; blame someone else for the cause of the disease.
The health worker's ideas about the so-called "ideal patient" can also complicate the process of communication. This concept includes the following characteristics: the patient's low awareness of medical issues, faith and lack of doubt in the strength and skills of the physician, the willingness to unquestioningly fulfill appointments, the ability to clearly state one's problem and complaints, the absence of hypochondria (fixation on the disease). The physician is usually aimed at an authoritarian style of interaction with the patient, and is not always ready for cooperation, for true partnership. Perhaps this is due to protection from professional "burnout", psychological fatigue. With the directive behavior of the health worker, and consequently, the dependent behavior of the patient, the physician takes full responsibility for the outcome of the treatment process, since he is convinced that a negative result will be considered as his mistake or a manifestation of incompetence.
Communication with patients is one of the main elements of the treatment process. Therefore, an important task of a medical worker is to understand the personality traits, life goals, attitudes and motives of a sick person, as well as the ability to predict the response to various situations that arise in the course of treatment.
Modern medical deontology is a complex of legal, professional and moral duties and rules of behavior of a doctor in relation to the patient, his relatives and friends, and colleagues. This is the doctrine of the doctor's duty to the patient and his relatives. Based on it, the relationship between health workers is determined. Medical deontology as a scientific discipline is the core basis of medical ethics.
The issues of education, professional training, deontology and medical ethics should occupy one of the leading places in shaping the personality of a qualified emergency physician.
Before setting out the main provisions of medical ethics and deontology, their application and use in the daily practical work of an emergency physician, it is necessary, at least in general terms, to characterize the features of the work of this specialist.
The profession of an emergency doctor is a heroic specialty. The work of an ambulance doctor can be fully and accurately performed only by an excellently and comprehensively trained general practitioner. An ambulance doctor, based on the characteristics of his work, should be fully inherent in the following qualities:
Good health, highly organized, balanced and mobile nervous system, sufficiently strong physical and psychological endurance;
Special professional medical observation, determined by well-developed sense organs: vision, hearing, smell, touch, taste sensations;
A high sense of optimism, which is based on a fairly rich practical experience and good knowledge of one's specialty;
The ability to remain calm, composure and constant readiness to solve new problems in the diagnosis and treatment of urgent pathological conditions in patients and victims in an unusual situation at any time of the day, in the presence of high nervous and mental stress;
High professional preparedness, namely: knowledge of all emergency conditions that may occur at the pre-hospital stage, the principles and methods of their recognition, the ability to quickly and efficiently carry out emergency medical measures, choose the best tactics;
The ability to quickly and easily get in touch with any patient and his relatives, despite the fact that the patient has a severe, sometimes incurable disease;
Possession of logical thinking and reasoning, the ability to convince the patient and relatives of the correctness of their conclusions;
The ability to understand the patient, instill in him faith in recovery, dispel his doubts and fears, support him under any circumstances, no matter how unfavorable they may be for the patient;
Exceptional discipline, modesty, cleanliness, high decency; special courtesy in relations with patients and their relatives;
Deep knowledge of the professional preparedness of their colleagues and paramedical staff; the formation and constant maintenance of the high authority of colleagues and nursing staff among patients and their relatives.
The listed features that characterize the emergency doctor cannot fully reflect his daily work.
Despite the complexity and great responsibility of the daily practice of an ambulance doctor, he needs to clearly and scrupulously follow the rules of medical ethics and deontology.
The work of an ambulance doctor is constantly associated with the examination and treatment of a large number of patients. Hence, the most important thing in the doctor's activity is to win the trust of the patient. Undoubtedly, the doctor should always be calm, polite, avoid arrogance and haste. The patient, in turn, will trust the doctor if he believes in his sincerity, conscientiousness, is convinced of his competence and qualifications, if he feels that the doctor understands him and is friendly towards him.
One of the important elements of medical ethics is the preservation of medical secrecy. A doctor upon graduation from a medical institute, taking the Oath of a doctor, makes a vow to always keep medical secrets. Particularly carefully and punctually, this vow must be observed by the emergency physician. By the nature of his activity, he has to talk not only with patients, but also with their relatives, people close to them, and neighbors. And in conversations with the latter, the ambulance doctor should be extremely careful, since even the closest relatives cannot always be informed in detail about the state of health of a newly examined patient. Academician N. N. Blokhin believes that a wide notification of acquaintances, and even relatives of the patient about the state of his health, when this is not necessary or is associated with the preservation of medical secrecy, is the real way to declassify it.
In the spirit of a pedantic attitude to the preservation of medical secrecy, it is necessary to educate all members of the ambulance team. The ambulance doctor should periodically remind members of his team that professional conversations after examining the patient should in no case be conducted in the apartment, in the kitchen, in the corridor, on the landing and stairs, since there is never a complete certainty that they are not may be accidentally or intentionally heard by unauthorized persons. The state of health of the patient must be very tactfully and briefly, without unnecessary details, reported only to his closest relatives in the absence of unauthorized persons.
The emergency doctor also needs to be very careful in formulating his report to the responsible doctor or shift supervisor about making a call, especially if he does this using the patient's home phone.
Performing a visit to the patient, the emergency doctor should never show the appearance that he has little time, a lot of other calls and he is in a hurry. This usually makes a very bad impression. The conversation between the doctor and the patient should proceed without any haste, in an atmosphere of goodwill, the initiator should be the doctor who directs it in the right direction. A frank conversation helps the patient to speak out, to open up. The conversation should be conducted in a language understandable to the patient, and correspond to the level of his knowledge and intelligence. The doctor should always strive to ensure that, carefully following the course of the conversation, make the patient to some extent an assistant capable of contributing to the diagnosis and the success of treatment.
An ambulance doctor should be aware that at present, due to the growth of the general culture and education of the population, an increase in some people's interest in medicine, especially due to concern for their health, as well as relatives and relatives, the number of "enlightened patients" has significantly increased , especially among the "militant dilettantes". In a conversation with such patients, the doctor needs to be especially sensitive and patient. Before them, the ambulance doctor acts as an authorized representative of medicine and patiently convinces them of the correctness of the diagnosis and the need for the prescribed treatment.
A conversation between an ambulance doctor and suspicious patients who already presuppose the presence of a serious and incurable disease should have a completely different character. With such patients, one should always talk about their illness with a certain degree of optimism. If possible, then such a patient should be accurately informed of the diagnosis of his disease, in a simple presentation, reveal the essence of this disease and thereby try to involve him in active participation in the treatment.
The ambulance doctor is obliged to pay constant attention to the relationship between the members of the ambulance team. There should be normal comradely relations between members of the brigade, which are built on mutual respect and maintaining the authority of each other, comradely mutual assistance. Such relationships determine a healthy psychological climate in the team, maintain a good cheerful mood among all its members. The ambulance doctor should understand that the arrogant and dismissive attitude of the doctor, the head of the team, towards junior and middle medical workers is especially intolerant. The facts are outrageous when a doctor refers to "you" and calls only by name a nurse, a nurse, a paramedic, a driver who are much older than him in age. This shows not only a disrespectful attitude towards a person, but also a misunderstanding of the important role that plays in ensuring the work of the ambulance brigade junior, middle and technical personnel.
It is known that one of the first duties of any doctor is to maintain the authority of his colleague. Unfortunately, there are still doctors who can tell the patient “You were not treated that way”, or “Yes, you have a completely different disease, you were incorrectly diagnosed”, or “Why were you operated on?” A well-mannered, highly qualified, knowledgeable ER doctor would never allow himself this. It is the duty of every physician to exercise reasonable tolerance for the opinion of his colleague. Attempts to create authority for themselves by belittling the authority of another doctor have never been successful.
An ambulance doctor who correctly, competently, in compliance with all the laws of honor, morality and medical ethics builds his work and relationships with colleagues, middle and junior medical staff, patients and relatives and observes all the basic principles and rules of medical deontology, as a rule, it is easy to work . If, in the event of an unfavorable outcome, all the rules of deontology were observed in the treatment of a seriously ill patient, then the relatives of the deceased often become defenders of the doctor who provided assistance. And vice versa, if these rules are not observed between the patient and relatives, on the one hand, and the doctor, on the other, a conflict may arise even in cases of completely correct treatment and recovery of the patient.
At the same time, one should not justify those patients who, having read popular scientific literature, became infected with self-confident skepticism, which greatly complicates the relationship of patients with doctors. The attitude of such a patient to the doctor often takes the form of rudeness and hostility. Here the doctor needs to show a resolute, albeit restrained in form, intolerance. One must be able to rebuff any manifestation of arrogance and disregard for the personality of the doctor on the part of patients.
An ambulance doctor should never despair, even in the most adverse circumstances. Based on professional training, he can always count on the best and find the right way out of the most difficult circumstances.
It should also be emphasized that the requirements for the professional training and responsibility of the emergency doctor have always been increased. His behavior at the bedside of the patient should serve as an example to follow. Quick in action, the doctor must be careful in his judgments and in no case be hasty in his conclusions and conclusions. He must observe all, without any exception, the rules of deontology in a conversation with a patient and during his examination.
In conclusion, it must be emphasized that the full possession of such qualities as modesty, crystal honesty, respect, mutual assistance and support allows the emergency doctor to fully comply with the requirements of medical deontology and medical ethics, and this, in turn, has a great assistance in his daily and difficult practical work.
ORGANIZATION OF EMERGENCY CARE
INTRODUCTION
Emergency medical care - the type and system of emergency medical care provided to patients with sudden acute diseases and exacerbations of chronic diseases in their places of residence: at home, in a hotel, hostel, etc.
Emergency medical care is provided around the clock by emergency departments of territorial medical institutions or associations for adults and children at the place of residence, and emergency doctors are called to the house for the above diseases and conditions.
The emergency department may be structural unit territorial medical institution (association) or an independent institution with direct subordination to local health authorities.
The emergency department is responsible for the following tasks:
Provision of emergency medical care in all cases of acute chronic diseases and their exacerbations, provision, according to indications (life-threatening conditions, etc.), of calling an ambulance team according to the profile of the disease (damage);
Organization, in necessary cases, of hospitalization of patients through an ambulance station or ambulance transport;
Ensuring continuity in work with district doctors and medical specialists in the treatment and monitoring of patients;
Timely notification of SES about cases of detected infectious diseases.
In the course of performing their duties, the emergency physician may encounter
with the development of conditions requiring or suggesting the possibility of resuscitation. Therefore, even before the arrival of the ambulance team, he must assess the state of the functions of vital organs and systems, and, if necessary, perform cardiopulmonary resuscitation (CPR).
Emergency physicians have the right to issue sick leaves for temporary disability for up to three days in the prescribed manner and prescriptions for medicines.
Emergency physicians are prohibited from conducting an examination for alcohol and drug intoxication, as well as issuing a forensic medical report.
The relationship between the functions of ambulance and emergency care in our country has a long and controversial history. The combination of both services contributed to the transfer of emergency care to the organizational rails of an emergency service, which is an ambulance, but at the same time diverted ambulance forces from performing direct tasks, led to delays in making calls and other adverse consequences, among which continuity was not the last place. in cooperation with local outpatient clinics. On the other hand, the separation of these services in the past and the transfer of emergency services to polyclinics did not ensure constant round-the-clock availability of emergency care, which ultimately became an additional burden on the ambulance service.
Transition to Methods economic management allowed to materially interest the medical staff of the prehospital stage in the quantity, quality and optimal results of their work. This, in turn, made it possible to organizationally distinguish between the tasks and functions of ambulance and emergency care.
Emergency medical care - a type and system of emergency medical care for patients and victims with conditions that threaten their life and health and injuries, provided at the scene of an accident: on the street, in public places, at home and on the way when the patient is taken to the hospital.
This does not mean at all that the ambulance teams, linear and specialized, do not provide care to the sick and injured at home in emergency conditions that threaten their lives. Interaction in the work of ambulance and emergency services exists constantly.
In conclusion, it should be emphasized that positive results have been achieved in the separation of emergency and emergency medical services with the transition to new methods of economic management. Continuity in the work of services and emergency medical care has increased. Emergency medical care approached the patients, began to be provided in a short time in terms of continuity and co-operation with specialists from polyclinics. The number of calls for emergency medical care has significantly decreased, which allowed her to fulfill her direct duties of providing emergency benefits to the sick and injured outside the apartment.
The objective of this guide is to systematize the experience accumulated in the country and, in particular, in St. Petersburg, the experience of the emergency service, separated from the ambulance, and the transformation of this experience into the property of the entire system of practical healthcare.
Similar information.
Modern medical deontology is a complex of legal, professional and moral duties and rules of behavior of a doctor in relation to the patient, his relatives and friends, and colleagues. This is the doctrine of the doctor's duty to the patient and his relatives. Based on it, the relationship between health workers is determined. Medical deontology as a scientific discipline is the core basis of medical ethics. The issues of education, professional training, deontology and medical ethics should occupy one of the leading places in shaping the personality of a qualified SMP doctor. The profession of an emergency doctor is a heroic specialty. The work of an ambulance doctor can be fully and accurately performed only by an excellently and comprehensively trained general practitioner.

The following qualities should be fully inherent in an ambulance doctor: 1. good health, a balanced and mobile nervous system, sufficiently strong physical and psychological endurance; 2. special professional medical observation, determined by well-developed sense organs: vision, hearing, smell, touch, taste sensations; 3. a high sense of optimism, which is based on a fairly rich practical experience and good knowledge of one's specialty; 4. the ability to remain calm, composure and constant readiness to solve new problems in the diagnosis and treatment of urgent pathological conditions in patients and victims in an unusual situation at any time of the day, in the presence of high nervous and mental stress;

5. high professional readiness, namely: knowledge of all emergency conditions that may occur at the pre-hospital stage, the principles and methods of their recognition, the ability to quickly and efficiently carry out emergency medical measures, choose the best tactics; 6. the ability to quickly and easily get in touch with any patient and his relatives, despite the fact that the patient has a severe, sometimes incurable disease; 7. possession of logical thinking and reasoning, the ability to convince the patient and relatives of the correctness of their conclusions; 8. the ability to understand the patient, instill in him faith in recovery, dispel his doubts and fears, support him under any circumstances, no matter how unfavorable they may be for the patient; 9. exclusive discipline, modesty, cleanliness, high decency; special courtesy in relations with patients and their relatives; 10. Formation and constant maintenance of the high authority of colleagues and nursing staff among patients and their relatives.

Despite the complexity and great responsibility of the daily practice of an ambulance doctor, he needs to clearly and scrupulously follow the rules of medical ethics and deontology. The work of an ambulance doctor is constantly associated with the examination and treatment of a large number of patients. Hence, the most important thing in the doctor's activity is to win the trust of the patient. Undoubtedly, the doctor should always be calm, polite, avoid arrogance and haste. One of the important elements of medical ethics is the preservation of medical secrecy. Particularly carefully and punctually, this vow must be observed by the emergency physician.

In the spirit of a pedantic attitude to the preservation of medical secrecy, it is necessary to educate all members of the ambulance visiting team. The ambulance doctor should periodically remind members of his team that professional conversations after examining the patient should in no case be conducted in the apartment, in the kitchen, in the corridor, on the landing and stairs, since there is never a complete certainty that they are not may be accidentally or intentionally heard by unauthorized persons. The state of health of the patient must be very tactfully and briefly, without unnecessary details, reported only to his closest relatives in the absence of unauthorized persons. The emergency doctor also needs to be very careful in formulating his report to the responsible doctor or shift leader about making a call, especially if he does this using the patient's home phone.

Performing a visit to the patient, the emergency doctor should never show the appearance that he has little time, a lot of other challenges, and he is in a hurry. This usually makes a very bad impression. The conversation between the doctor and the patient should proceed without any haste, in an atmosphere of goodwill, the initiator should be the doctor who directs it in the right direction. A frank conversation helps the patient to speak out, to open up. The conversation should be conducted in a language understandable to the patient, and correspond to the level of his knowledge and intelligence. The doctor should always strive to ensure that, carefully following the course of the conversation, make the patient to some extent an assistant capable of contributing to the diagnosis and the success of treatment.

An ambulance doctor should be aware that at present, due to the growth of the general culture and education of the population, an increase in some people's interest in medicine, especially due to concern for their health, as well as relatives and relatives, the number of "enlightened patients" has significantly increased , especially from among the "militant amateurs". In a conversation with such patients, the doctor needs to be especially sensitive and patient. Before them, the ambulance doctor acts as an authorized representative of medicine and patiently convinces them of the correctness of the diagnosis and the need for the prescribed treatment.

A conversation between an ambulance doctor and suspicious patients who already presuppose the presence of a serious and incurable disease should have a completely different character. With such patients, one should always talk about their illness with a certain degree of optimism. If possible, then such a patient should be accurately informed of the diagnosis of his disease, in a simple presentation, reveal the essence of this disease and thereby try to involve him in active participation in the treatment.

Analysis of cases from the practice of an ambulance doctor As a rule, the ambulance either does not have its own “workforce” or it is not enough: the team is mostly women. When deciding on hospitalization, such a dialogue often arises: - Look for men, we have no one to carry! We don't have anyone either. You have a driver, we will pay him! He can't leave the car! Verbal duel, as a rule, leads to nothing. Try to start the conversation differently: “The patient needs to be carried on a stretcher, you see, we have only women, maybe you can help us find someone, because we don’t know anyone here.” This is how the conversation should go. No categoricalness, no "stubbornness", a friendly, calm tone. Then you can count on success.

Here is another situation: when transporting on a stretcher from some floor, relatives (surrounding) may be perplexed why the patient is carried “feet forward”, because he is still alive? In this case, the doctor or any member of the team should calmly, tactfully explain that this is not “feet forward”, but “feet down”. Because if you take it head first, then on the stairs it will be head down, which is not safe for a seriously ill patient. That is why "feet down" and not feet forward.

"Ambulance" is in a special position. Sometimes they call her without receiving a referral to the hospital from “their” district doctor or without waiting today for a doctor from the clinic ... But you never know what else! Even a conversation with the dispatcher prior to the arrival of the brigade can drive a sick person “out of himself”. And all the accumulated negative emotions will be thrown out on the one who is available, and from whom you can get the most specific and real help. But here you are “attacked” with a stream of claims to which you have nothing to do. Start immediately "defend" when the patient or relatives are still hot? This energy will involuntarily be transferred to you (mirror effect), you will get involved in a conflict, and it is possible that you will suffer from it. How to be? There is such an approach. Ask the essence of the claim (knowing very well that it is not for you) to state it again, explaining that you did not understand something. (Just don’t interrupt the patient, let him speak. The time spent on this will pay off by preventing a conflict, maybe even a complaint, which will then take much more time to resolve and not one, but several people. Do not forget to reflect this situation in the call card). You will notice that there will be less emotions. In extreme cases, you can ask to repeat some part of the entire claim again. The conversation will be very calm. You have given the patient the opportunity to "let off steam." This is just one way to avoid conflict.

It is known that one of the first duties of any doctor is to maintain the authority of his colleague. Unfortunately, in our country there are still doctors who can tell the patient: “You were not treated like that,” or “Yes, you have a completely different disease, you were diagnosed incorrectly,” or “Why were you operated on?” A well-mannered, highly qualified, knowledgeable ER doctor would never allow himself this. It is the duty of every physician to exercise reasonable tolerance for the opinion of his colleague. Attempts to create authority for themselves by belittling the authority of another doctor have never been successful.

The ambulance doctor is obliged to pay constant attention to the relationship between the members of the ambulance team. There should be normal comradely relations between the members of the brigade, which are built on mutual respect and maintaining the authority of each other, comradely mutual assistance. Such relationships determine a healthy psychological climate in the team, maintain a good cheerful mood among all its members. An ambulance doctor should understand that the arrogant and dismissive attitude of the doctor, the head of the team, towards junior and middle medical workers is especially intolerant. It is unacceptable when an EMS doctor refers to "you" and calls only by name a nurse, a nurse, a paramedic, a driver who are much older than him in age. This shows not only a disrespectful attitude towards a person, but also a misunderstanding of the important role that junior, middle and technical personnel play in ensuring the work of an ambulance brigade.

Who is morally responsible for human life and health? The answer to it depends on the system of values in which life is considered, or rather, at what level of the value hierarchy: In the system of "human society", the state obviously bears moral responsibility for human life and health. It should ensure the possibility of survival of each person and the conditions for maintaining his health. To some extent, these functions are performed by all social institutions

In the “human social group” system, the responsibility for the health and life of a person obviously lies with the members of the group. In this sense, such a group as the family is indicative. This responsibility is less obvious in those groups that are called labor collectives. in terms of our consideration, there is a phenomenon of mutual responsibility of each for each.But if in ordinary interpersonal relationships this fact remains unconscious until something happens, then the picture is completely different if one of the interacting people is a doctor. human responsibility for the life and health of a partner is strengthened by professional duty, duties assigned to him by society.Therefore, it seems that the only people who bear moral responsibility for the life and health of others are medical workers.

Who is responsible for the life and health of a person, except for those with whom he interacts? The answer is simple man himself. But this simplicity turns out to be inaccessible to the moral consciousness of many. Taking care of one's own health and the instinct of self-preservation is one thing, but responsibility to others for one's life and health is another. This is the norm of morality, which has not yet acquired an imperative character. A dependent position on the issue of one's own health leads, in fact, to new diseases. For medical professionals, the position of the patient in relation to his health is not indifferent, moreover, it is fundamentally important for the entire course of treatment. Therefore, the very principles of medical ethics, even if strictly observed, do not yet guarantee that morality will contribute to the success of treatment.

Principles of medical morality principle do no harm; principle do good; the principle of caring for the patient; the principle of respect for patient autonomy; the principle of maintaining medical secrecy; the principle of a differentiated approach to reporting a diagnosis; iatrogenic exclusion principle.

The principle of do no harm According to B.G. Yudin, the concept of harm from the point of view of a doctor can be considered in four senses: a) harm caused by inaction (failure to provide assistance); b) damage caused by negligence or malice; c) harm caused by unskilled (or thoughtless) actions; d) harm caused by actions necessary in a given situation. For example, untimely provision of assistance: A teenager was admitted to the traumatological department, who was injured as a result of a traffic accident (he was hit by a car while riding a bicycle). The doctor on duty had some time left before the shift and he decided not to help transfer the patient to the doctor who was changing him. The doctor who came on duty needed time to prepare for the implementation of therapeutic measures. As a result of untimely assistance, the child died. A fatal accident was the fact that the teenager was the son of a doctor who did not help the victim and did not even approach him. How to evaluate the act of a doctor? What is the punishment for the doctor? Or can it be considered already punished? It is obvious that there is: a) the fact of failure to provide assistance to those in need of it, which is no longer subject to ethical, but legal regulation, and b) if the patient was admitted when the doctor's working hours had already ended, the fact of not providing assistance is the subject of an ethical assessment, the principle of no harm is violated, but the principle of justice is also violated.

The principle of doing good It is possible to resolve the conflict between the doctor's values and the patient's values, but how this is achieved will depend on the doctor's model of communication with the patient. There are four main models of interaction between a doctor and a patient: paternalistic, collegial, contractual and technocratic. The first (paternalistic) is the most common and implies that the doctor is wiser than the patient, knows more and must make decisions himself. According to this model, the conflict of values is resolved in favor of the doctor. In the collegial model, there are high requirements for patient awareness, which ensures cooperation with the doctor in contentious issues. In the contract model, not only the patient, but also the doctor is morally protected. The technocratic model generally tries to eliminate the ethical issue, since the doctor acts as a mechanic who corrects a breakdown, i.e. participates in the treatment process only with his knowledge and skills, but without a personal component. Such a model also has the right to exist, but with a developed service of social workers.

The Principle of Respect for Patient Autonomy The principle of respect for patient autonomy is one of the most difficult principles in medicine. It lies in the fact that the patient himself must give consent to the treatment, moreover, it must be informed, i.e. the doctor must offer the patient all the options for assistance that he can provide with the justification and prediction of the consequences. This in itself can be problematic, and patients are often guided by non-medical considerations in choosing a treatment option.

The reasons leading to the violation of the patient's rights by the medical personnel of the EMS: 1st level ("horizontal") - the prerequisites for errors arise and are realized at the level of the medical workers themselves due to: ignorance of these rights; failure to comply with known requirements related to the observance of the patient's rights, including the achievement of informed voluntary consent to medical intervention; specific features of the work of the medical staff of the ambulance service. 2nd level ("vertical") - when erroneous recommendations or command instructions become the cause of violations of the patient's rights officials, orders (often outdated) carried out by doctors or paramedics (the so-called "commission errors").

The rights of persons who have applied to the EMS service To respectful and humane treatment by medical and service personnel To examination, treatment and maintenance in conditions that meet sanitary and hygienic requirements To hold, at his request, a consultation and consult other specialists (or) medical intervention, available methods and means

The rights of persons who applied to the EMS service To keep confidential information about the fact of applying for medical care, about the state of health, diagnosis and other information obtained during his examination and treatment To informed voluntary consent to medical intervention, the patient must be warned about possible complications during conducting medical intervention To compensate for damage in case of harm to his health during the provision of medical care To refuse medical intervention.

Consent and Refusal of Patients from the Assistance of the EMS Service 1. When providing emergency care, oral consent of the patient for medical intervention must be obtained. 2. When providing SMP to persons under the age of 15, the consent of a parent or guardian is required. 3. In cases where the patient’s condition does not allow him to express his will or it is not possible to obtain the consent of the parent (guardian) in relation to persons under 15 years of age, and medical intervention is urgent, the issue of its implementation is decided by the doctor (paramedic) of the SMP with a mark in medical documentation and subsequent informing the administration of the institution about this fact. The patient's refusal to provide assistance is recorded in the documentation in the prescribed form. In these cases, in the event of death or harm to health, medical workers are not responsible.

4. The provision of medical care without the consent of the patient is allowed in relation to persons suffering from diseases or in a state that poses a danger to others. 5. The prior consent of the patient is excluded in the following cases: In case of incompetence of the patient (inadequate consciousness - alcohol intoxication, coma, psychosis, etc.) Urgency of action (cardiopulmonary resuscitation and other critical conditions). In these cases, the issue of providing assistance is decided by the doctor himself, if possible, involving specialists. A note is required in the documentation and informing the administration of the institution where the patient is delivered.

Types of responsibility of medical workers Directly or indirectly, all types of responsibility, except moral, are included in legal responsibility, which can be defined as state coercion to fulfill the requirements of law. Administrative liability is a type of legal liability for an administrative offense (offence), which is not regarded as strictly as the Criminal Code does. Disciplinary responsibility - a form of influence on offenders labor discipline as disciplinary action: remark, reprimand, dismissal on the appropriate basis. Civil, or civil law, liability is a type of legal liability in which measures of influence established by law or an agreement are applied to the offender. Criminal liability is a type of liability that is regulated by the Criminal Code.


Group A “Violations of moral and ethical rules” includes: violations of elementary norms of culture and professional behavior; conflict relations between SMP workers; mutual confrontation between the EMS doctor and the patient, provoked by: the EMS team or the patient, and / or his relatives; mutual confrontation between employees of the SMP and other medical and preventive institutions (HCF), provoked by: health workers of the SMP, health workers of health facilities; some types of iatrogenic (therapeutic and psychological).

The doctor of the ambulance team is responsible in accordance with the procedure established by law: 1. For the professional activities carried out in accordance with the approved industry regulations, rules and standards for the medical personnel of "Ambulance". 2. For illegal actions or omissions that caused damage to the patient's health or his death.


LEGAL DOCUMENTS OF THE FEDERAL LEVEL Constitution of the Russian Federation (Articles 41, 71, 72, 73) "Fundamentals of the legislation of the Russian Federation on the protection of the health of citizens" dated July 22, 1993 N the federal law RF “On the ambulance service and the status of its employees”.

"Fundamentals of the legislation of the Russian Federation on the protection of the health of citizens" dated July 22, 1993 N Article 54. The right to engage in medical and pharmaceutical activities: Persons who have received higher or secondary medical and pharmaceutical education in the Russian Federation have the right to engage in medical and pharmaceutical activities in the Russian Federation. Federations that have a diploma and a special title, and for engaging in certain types of activities, the list of which is established by the Ministry of Health of the Russian Federation, also a specialist certificate and license. A specialist certificate is issued on the basis of a postgraduate vocational education(postgraduate study, internship, residency), or additional education (advanced training, specialization), and a screening test conducted by commissions of professional medical and pharmaceutical associations on the theory and practice of the chosen specialty, legislation in the field of protecting the health of citizens. During the period of their studies in institutions of the state or municipal healthcare system, doctors have the right to work in these institutions under the supervision of medical personnel, responsible for their professional training. Students of higher and secondary medical educational institutions are allowed to participate in the provision of medical care to citizens in accordance with training programs under the supervision of medical personnel responsible for their professional training, in the manner established by the Ministry of Health of the Russian Federation. Persons illegally engaged in medical and pharmaceutical activities bear criminal liability in accordance with the legislation of the Russian Federation.

Federal Law of the Russian Federation "On the ambulance service and the status of its employees". Article 1 "Basic concepts": Emergency medical specialist - a doctor who has a certificate in the specialty "emergency medical care" and additional training in any specialty (pediatrics, psychiatry, cardiology, anesthesiology, toxicology, neurology, etc.). ). Article 15 "Admission of an ambulance doctor to professional activities": carried out on the basis of the federal regulation "On the admission of specialists to work in the ambulance service." Advanced training of an emergency medical doctor is carried out at least once every 5 years on mandatory cycles of general improvement in the specialty "emergency medical care" in accordance with programs approved by the Ministry of Health and social development Russian Federation, in institutions licensed for the right to study in this specialty.

Normative documents of the Federal level Organizing Orders of the Ministry of Health of the Russian Federation for emergency medical care. Related orders of the Ministry of Health of the Russian Federation concerning some aspects of the activities of the EMS service. Decrees of the Government of the Russian Federation. Decrees of the relevant ministries and departments of the Russian Federation, instructional letters, guidelines, clarifications, etc.

Organizing documents for the NSR. Order of the Ministry of Health of the Russian Federation 179 dated (ed. dated) "On approval of the Procedure for the provision of emergency medical care"

Organizing documents for the NSR. Order of the Ministry of Health of the Russian Federation 445n dated "On approval of the requirements for completing medicines and medical products for the installation of an ambulance team" Emergency"

Organizing documents for the NSR. Order of the Ministry of Health of the Russian Federation 942 dated "On approval statistical toolkit stations (departments), emergency hospitals" (together with "Instructions for filling out the industry statistical reporting form N 40" Report of the station (department), emergency hospitals "," Instructions for filling out the accounting form N 109 / y "Call record log ambulance", "Instructions for filling out the registration form N 110 / y "Card for calling an ambulance", "Instructions for filling out the registration form N 114 / y "Accompanying sheet of the station (department) of ambulance and a coupon for it", " Instructions for filling out the registration form N 115 / y "Diary of the work of an ambulance station") Decree of the Government of the Russian Federation N 101 dated (ed. from) "On the working hours of medical workers depending on their position and (or) specialty" IX. Stations (departments) of emergency medical care, stations (departments) of emergency and emergency medical care, departments of mobile emergency and advisory medical care of regional, regional and republican hospitals

Order of the Ministry of Health and Social Development of the Russian Federation 115n dated "On Approval of the Procedure for Providing Medical Assistance to the Population of the Russian Federation in Diseases of the Eye, Its Adnexa and Orbit" (together with the "Procedure for Providing Emergency Medical Care to the Population of the Russian Federation in Acute Diseases and Conditions of the Eye, Its Adnexa and Orbit" ) Order of the Ministry of Health and Social Development of the Russian Federation 966n dated "On approval of the procedure for providing medical care to patients with urological diseases" (together with the "Procedure for the provision of planned medical care to persons with urological diseases", "The procedure for providing emergency medical care to patients with urological diseases") Order of the Ministry of Health and Social Development of the Russian Federation 599n dated "On approval of the procedure for the provision of planned and emergency medical care to the population of the Russian Federation in diseases of the circulatory system of a cardiological profile" Letter of the Ministry of Health and Social Development of the Russian Federation 15-4 / 10 / from "On the direction of the methodological letter of the Ministry of Health and Social Development of the Russian Federation "Primary and resuscitation first aid to newborn children” Appendix 6 primary resuscitation newborn"

The rights of the doctor of the ambulance team. 1. If the patient refuses medical care and hospitalization, offer him, and if he is incapacitated, his legal representatives or relatives to confirm the refusal in writing in the "Call Card". 2. Allow relatives to accompany the patient (injured) in an ambulance. 3. To make proposals on improving the work of ambulance teams, improving the working conditions of medical personnel. 4. Improve your qualifications as an EMS specialist at least once every 5 years, pass certification and re-certification in the specialty in the prescribed manner. 5.Participate in production meetings, scientific and practical conferences, symposia.

The doctor of the ambulance team is obliged to: 1. Ensure the immediate departure of the team after receiving a call and its arrival at the scene of the incident within the established time limit in the given territory. 2. Provide emergency medical care to the sick and injured at the scene and during transportation to hospitals. 3. To administer medicines to patients and injured for medical reasons, to stop bleeding, to carry out resuscitation in accordance with approved industry norms, rules and standards for paramedical personnel for the provision of emergency medical care. 4. Be able to use the available medical equipment, master the technique of applying transport splints, dressings and methods of conducting basic cardiopulmonary resuscitation. 5. Own the technique of taking electrocardiograms. 6. Know the location of medical institutions and the service areas of the station. 7. When transporting a patient, be next to him, providing the necessary medical care. 8. If it is necessary to transport a patient in an unconscious state or in a state of alcoholic intoxication, inspect for the detection of documents, valuables, money indicated in the call card, hand them over to the admission department of the hospital with a mark in the direction against the signature of the staff on duty. 9. When providing medical assistance in emergency situations, in cases of violent injuries, act in accordance with the procedure established by law. 10. Ensure infectious safety 11. Inform the administration of the EMS station about all emergencies that occurred during the call. 12. At the request of the employees of the Department of Internal Affairs, stop to provide emergency medical care, regardless of the location of the patient (injured).

Responsibility of medical workers of the ambulance service for violation of the rights of citizens 1. Medical workers of the ambulance service are liable in accordance with the legislation of the Russian Federation if they perform their duties in bad faith, resulting in harm to the health of citizens or their death. 2. Unreasonable refusal to service a call is the basis for termination employment contract. 3. The doctor of the mobile ambulance team is responsible for the organization and quality of work of the ambulance team in accordance with the approved industry norms, rules and standards for medical personnel of the ambulance service.

Responsibility for encroachment on the life or health of EMS workers Encroachment on the life or health of EMS workers on duty official duties are punished according to the norms in accordance with the criminal legislation of the Russian Federation. In the event of a threat to the life or health of EMS personnel, medical assistance to patients can only be provided in the presence of representatives of law enforcement agencies, who must guarantee the safety of EMS workers.

When a wise man was asked from whom he learned good manners, he replied: “From the ill-mannered. I avoided doing what they do." And, finally, the wonderful thought of the French encyclopedist Denis Diderot: “It is not enough to do good, you must do it beautifully.”


Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted on http://www.allbest.ru/
abstract
On the topic: "Speech skills in the work of a medical worker"
Plan
1. Communication and its importance in medical activities
2. Features of relationships in medical activities
3. Types of communication
4. Health worker tactics
5. Features of the personality of a medical worker
6. Paramedic and patient, principles of communication with the patient
7. The role of the paramedic in communicating with the patient
List of used literature
I. Communication and its knowledgechivalry in medical activity
Communication -multifaceted process of developing contacts between people.
Communication plays an important role in the life and work of people. Without communication, it is impossible, for example, to develop culture, art, and the standard of living; only through communication, the accumulated experience of generations of the past is passed on to new generations. The topical issue today is the communication between the health worker and the patient. Many of us have been to a hospital, clinic, or health care facility where each of us interacted with a doctor or nurse. But has anyone thought how much this communication affects us, or rather, the course of our disease, and how a health worker can improve our condition? Of course, we can say that everything depends on the medicines that the doctor prescribes and the nurse gives us, the medical procedures are also prescribed by the doctor, but this is not all that is necessary for a complete recovery. The most important thing is the right attitude, which depends on the mental and emotional state of the patient. The attitude of the health worker has a huge impact on the patient's condition. And if the patient is satisfied, for example, with a conversation with a doctor who listened to him carefully, in a calm atmosphere and gave him appropriate advice, then this is already the first step towards recovery. Further in my essay, I will try to reveal in more detail the psychology of communication between a medical worker and a patient.
2. Relationship featuresin medical activities
The psychological characteristics of the patient in terms of therapeutic relationships and interactions come into contact with the psychological characteristics of the medical worker. In addition, persons involved in contact with the patient may be a doctor, psychologist, nurse, social worker.
In medical activity, a special connection is formed, a special relationship between medical workers and patients, these are relations between a doctor and a patient, a nurse and a patient. According to I. Hardy, the connection “doctor, sister, patient” is formed. Daily medical activity is connected with psychological and emotional factors in many nuances.
The relationship between doctor and patient is the basis of any medical activity. (I. Hardy).
The purpose of contacts between a medical worker and a patient is medical assistance provided by one of the participants in communication in relation to another. Such relationships are determined to a certain extent by the conditions in which medical activities are carried out. Based on the main goal of therapeutic interaction, one can assume the ambiguity of the importance of contacts in the system of interaction between a health worker and a patient. However, it should not be understood that there is an interest in such interaction only on the part of the patient. The health worker, in theory, is no less interested in helping the patient, because this activity is his profession. The health worker has his own motives and interests to interact with the patient, which allowed him to choose the medical profession.
In order for the process of the relationship between the patient and the medical worker to be effective, it is necessary to study the psychological aspects of such interaction. Medical psychology is interested in the doctor's motives and values, his idea of an ideal patient, as well as certain expectations of the patient himself from the process of diagnosis, treatment, prevention and rehabilitation, the behavior of a paramedic or nurse.
We can talk about the importance for the effective and conflict-free interaction of the patient with health workers of such a concept as communicative competence, i.e. the ability to establish and maintain the necessary contacts with other people. This process implies the achievement of mutual understanding between communication partners, a better understanding of the situation and the subject of communication. It should be noted that communicative competence is a professionally significant characteristic of a doctor and a nurse. However, despite the fact that in a clinic the patient is forced to seek help from a doctor, communicative competence is also important for the patient himself.
With good contact with the doctor, the patient recovers sooner, and the treatment used has a better effect, much less side effects and complications.
One of the foundations of medical activity is the ability of a health worker to understand a sick person.
In the process of medical activity, an important role is played by the ability to listen to the patient, which seems necessary for the formation of contact between him and the health worker. The ability to listen to a sick person not only helps to identify and diagnose the disease to which he may be susceptible, but the listening process itself has a favorable interaction on the psychological contact between the paramedic and the patient.
It is important to note that it is necessary to take into account the characteristics (professionalism) of the disease when in contact with the patient. These are, for example, patients with diseases of the cardiovascular system, gastrointestinal tract, respiratory organs, kidneys, etc. And often their painful conditions require long-term treatment, which also affects the relationship between the health worker and the patient. A long separation from the family and the usual professional activities, as well as anxiety about the state of one's health, cause a complex of various psychogenic reactions in patients.
But not only these factors affect the psychological atmosphere and the patient's condition. As a result, psychogeny can complicate the course of the underlying somatic disease, which, in turn, worsens the mental state of patients. And, besides, in the therapeutic departments for examination and treatment there are patients with complaints about the activity of internal organs, often not even suspecting that these somatic disorders are of a psychogenic nature.
In the clinic of internal diseases, specialists deal with somatogenic and psychogenic disorders. In both cases, patients express a large number of different complaints and are very wary of their condition.
Somatogenically conditioned mental disorders often occur in anxious and hypochondriacal patients with hypochondriacal fixation on their condition. In their complaints, in addition to those caused by the underlying disease, there are many neurosis-like ones. For example, complaints of weakness, lethargy, fatigue, headache, sleep disturbance, fear for one's condition, excessive sweating, palpitations, etc. There are even various affective disorders in the form of intermittent anxiety and melancholy of varying severity. Such disorders are often observed in patients with hypertension, coronary heart disease, in persons suffering from gastric ulcer and duodenal ulcer. And neurosis-like symptoms can often mask the clinic of the underlying disease. As a result of this phenomenon, sick people turn to specialists of various profiles.
In everyday life, one often hears about the "good" or "correct" treatment of the patient. And in contrast to this, unfortunately, one hears about "heartless", "bad" or "cold attitude towards sick people". It is important to note that various kinds of complaints, emerging ethical problems indicate the lack of the necessary psychological knowledge, as well as the practice of appropriate communication with patients on the part of health workers. Differences in the views of the health worker and the patient. communication paramedic patient medical
Differences in the points of view of the health worker and the patient may be due to their social roles, as well as other factors.
For example, a paramedic tends to look, first of all, for objective signs of a disease. He tries to limit the history to further determine the prerequisites for further somatic research, etc. And for the patient, his subjective, personal experience of the disease is always in the center of attention and interests. In this regard, the doctor must consider these subjective feelings as real factors. He should even try to feel or catch the experiences of the patient, understand and evaluate them, find the causes of anxieties and experiences, support them. positive sides, also use them to more effectively assist the patient in his examination and treatment.
The differences in all the views and points of view of the paramedic (nurse) and the patient are quite natural and predetermined, in this situation, by their different social roles. However, the paramedic (nurse) needs to ensure that these differences do not turn into deeper contradictions. Since these contradictions can jeopardize the relationship between the medical staff and the patient, and thereby making it difficult to provide assistance to the patient, complicating the treatment process.
To overcome differences in views, the health worker needs not only to listen with great attention to the patient, but also to try to understand him as best as possible. What happens in the soul, thoughts of a sick person? The paramedic must respond to the patient's story with all his knowledge, reason in the fullness of his personality. The response of the health worker should be a resonance to what they hear.
3. Common typesnia
The following types of communication are distinguished (Samygin. S.I.):
1. "Mask Contact" This is formal communication. There is no desire to understand and take into account the personality traits of the interlocutor. Using the usual masks (politeness, courtesy, modesty, compassion, etc.). A set of facial expressions, gestures, standard phrases that allow you to hide true emotions, attitude towards the interlocutor.
As part of the diagnostic and therapeutic interaction, it manifests itself in cases of little interestparamedicor patient in the results of the interaction. This can happen, for example, during a mandatory preventive examination, in which the patient feels dependent, andparamedic-not havingnecessary data for conducting an objective and comprehensive examination and making a reasonable conclusion.
2. Primitive communication. They evaluate the other person as a necessary or interfering object, if necessary, they actively come into contact, if it interferes, they repel.
This type of communication can be found in manipulative communicationparamedicand the patient in cases where the purpose of contactingparamedicy becomes receiving any dividends. For example, a sick leave certificate, a certificate, a formal expert opinion, etc. On the other hand, the formation of a primitive type of communication can occur at willparamedica - in cases where the patient turns out to be a person on whom well-being may dependparamedica. For example, a leader. Interest in the contact participant in such cases disappears immediately after the desired result is obtained.
3. Formal role communication. Both the content and means of communication are regulated, and instead of knowing the personality of the interlocutor, they manage with knowledge of his social role.
A similar choice of the type of communication from the outsideparamedicand may be due to professional overload. For example, at the districtparamedicat the reception.
4. Business conversation. Communication, taking into account the peculiarity of the personality, character, age, mood of the interlocutor, while focusing on the interests of the case, and not on possible personal differences.
When communicatingparamedicand with the patient, this kind of interaction becomes unequal.Paramedicconsiders the patient's problems from the standpoint of his own knowledge, and he is inclined to take directive decisions without coordination with another participant in communication and an interested person.
Diagnostic and therapeutic interaction does not imply such contact, at least, due to the professional orientation, it does not provide for the confession of a medical worker.
6. Manipulative Communication. Just like primitive communication, it is aimed at extracting benefits from the interlocutor using special techniques. Many may be familiar with a manipulative technique, more commonly referred to as "hypochondriacization of the patient."
Its essence lies in the presentation of the conclusionparamedicabout the state of health of the patient in line with a clear exaggeration of the severity of the disorders found. The purpose of such manipulation can be:
- decrease in patient expectations for the success of treatment due to the avoidance of responsibility by the health worker in the event of an unexpected deterioration in the patient's health
- demonstration of the need for additional and more qualified interventions on the part of the health worker in order to receive remuneration.
Communication between a health worker and a patient can, in principle, be called forced communication. One way or another, but the main motive for meetings and conversations of a sick person with a health worker is the appearance of health problems in one of the participants in such an interaction. On the part of the paramedic and nurse, there is a compulsion to choose the subject of communication, which is due to his profession, his social role. And if the patient's appeal to the doctor is, as a rule, due to the search for medical care, then the doctor's interest in the patient is explained by considerations of his professional activity.
The interaction between patient and paramedic is not something forever given. Under the influence of various circumstances, they can change, they can be influenced by a more attentive attitude towards the patient, a deeper attention to his problems. At the same time, they themselves a good relationship health worker and patient contribute to greater effectiveness of treatment. Conversely, positive treatment outcomes improve the interaction between patient and provider.
Currently, many experts believe that it is necessary to gradually remove such concepts as “sick” from the process of communication and vocabulary, replacing the concept of a patient, due to the fact that the very concept of “sick” carries a certain psychological burden. And appeals to sick people like: “How are you, sick?” It is unacceptable to use, and it is necessary to try everywhere to replace such appeals to the patient with appeals by name, first name, patronymic, especially since the name itself for a person, his pronunciation, is psychologically comfortable.
4. Health worker tactics
Communication with the patient is an essential element of the treatment process.
The art of taking an anamnesis is not an easy art. In the language of psychologists, this is a guided conversation designed to collect anamnestic data, and the conversation should be controlled imperceptibly. The patient with whom the conversation is being conducted should not feel this. In the process of collecting an anamnesis, he should give the impression of a casual conversation. At the same time, the paramedic needs to assess the seriousness of complaints, the manner in which they are presented, to separate the main from the secondary, to verify the reliability of the testimony, without offending the patient with distrust, to help remember without inspiring. All this requires a lot tact , especially when it comes to clarifying the state of mind, mental trauma, which play a large role in the development of the disease.
When questioning a patient, one should always take into account his cultural level, degree of intellectual development, profession and other circumstances. Empty, meaningless words, indulgence in the unreasonable whims and demands of some patients should be avoided. In other words, it is impossible to offer a standard form of conversation between a health worker and a patient. This requires ingenuity and creativity.
Particular attention should be paid to elderly patients and children. The attitude of a paramedic or nurse to a child, a patient of mature age and an old man, even with the same illness, should be completely indifferent, which is due to age characteristics these patients.
5. Peculiaritiesthe identity of the medical worker
It should be noted that the prerequisite for the emergence of positive psychological relationships and trust between health workers and patients is the qualifications, experience and art of the paramedic and nurse. At the same time, the result of expanding and deepening information in modern medicine is the increased importance of specialization, as well as the creation of various branches of medicine aimed at certain groups of diseases depending on localization, etiology and methods of treatment. It can be noted that in this case, specialization carries with it a certain danger of a narrowed view of the paramedic on the patient.
Medical psychology itself can help offset these negative aspects of specialization through a synthetic understanding of the patient's personality and body. And qualification is only a tool, the greater or lesser effect of the use of which depends on other aspects of the paramedic's personality. We can note the definition of the patient's trust in the paramedic, given by Gladkiy:
"Confidence inparamedicy is the positive dynamic attitude of the patient toparamedicy expressing the conditioned expectation by previous experience thatparamedichas the ability, means and desire to help the patient in the best possible way.
For the manifestation of trust in a health worker, the first impression that a patient has when meeting with him matters. At the same time, the actual facial expressions of a medical worker, his gestures, tone of voice, facial expressions arising from the previous situation and not intended for the patient, the use of slang speech turns, as well as his appearance are important for a person. For example, if a sick person sees an untidy, sleepy paramedic, then he may lose faith in him, often believing that a person who is not able to take care of himself cannot take care of others. Various behavioral and appearance Patients tend to forgive only providers they already know and trust.
A health worker gains the trust of patients if, as a person, he is harmonious, calm and confident, but not arrogant. Basically, in cases where his demeanor is persistent and resolute, accompanied by human participation and delicacy. It should be noted that when making a serious decision, the paramedic must imagine the results of such a decision, its consequences for the patient's health and life, and increase his sense of responsibility.
Special requirements for the health worker are the need to be patient and self-controlled. He must always consider various possibilities for the development of the disease and not consider ingratitude, reluctance to be treated, or even a personal insult on the part of the patient if the patient's condition does not improve. There are situations when it is appropriate to show a sense of humor, however, without a hint of mockery, irony and cynicism. Such a principle as “laugh with the patient, but never at the patient” is known to many. However, some patients cannot stand humor even with good intentions and understand it as disrespect and humiliation of their dignity.
There are facts when people with unbalanced, uncertain and absent-minded manners gradually harmonized their behavior in relation to others. This was achieved both through their own efforts and with the help of other people. However, this requires certain psychological efforts, work on oneself, a certain critical attitude towards oneself, which for a health worker is and should be taken for granted.
It should be noted that a medical worker - a young specialist, about whom patients know that he has less life experience and less qualifications, is in the search for the trust of patients and is in a more disadvantageous position compared to his older colleagues with work experience. But a young specialist can be helped by the realization that this shortcoming is transitory, which can be compensated by conscientiousness, professional growth and experience.
It should be noted that the personal shortcomings of a health worker may lead the patient to think that a paramedic or nurse with such qualities will not be conscientious and reliable in the performance of their direct duties.
In general, the balanced personality of a health worker is for the patient a complex of harmonic external stimuli, the influence of which takes part in the process of his treatment, recovery and rehabilitation. A health worker can educate and shape his personality, including by observing the reaction to his behavior directly. Let's say, according to the conversation, assessment of facial expressions, gestures of the patient. Also indirectly, when he learns about the view of his behavior from his colleagues. Yes, and he himself can help his colleagues guide them towards more effective psychological interaction with patients.
6. Paramedicand the patient, principles of communication with the patient
The position and role of the paramedic is becoming more important in our time. The patient seeks understanding and support from him. The work of a paramedic is associated not only with great physical exertion, but also with great emotional stress. The latter occurs when communicating with patients who are distinguished by increased irritability, painful exactingness, touchiness, etc. It is very important to establish contact with the patient. The paramedic is constantly among the patients, therefore his clear actions and professional performance, his benevolent, warm attitude towards the patient have a psychotherapeutic effect on him. The paramedic should be able to show understanding of the difficulties and problems of the patient, but should not seek to solve these problems.
In contact between the paramedic and the patient, the personality of the paramedic is of great importance. He can love his profession, have excellent technical data and skills, however, if, due to personal characteristics, he often conflicts with patients, his professional qualities do not give the desired effect. The path to true mastery is always long and difficult. Therefore, it is necessary to develop the necessary style of work and master the art of a beneficial effect on patients.
7. Roleparamedic in communication with the patient
The topic covered by me in this essay is of great importance for health workers, especially for me, the future paramedic. Therefore, this topic is interesting to me, and when writing an essay, I made certain conclusions for myself that will help me in my future professional activities.
As in ordinary life, so in medical activities, there is communication. In both cases, it has a certain meaning and psychological characteristics. In medical activities, there are several types of communication between a health worker and a patient. And it depends only on the health worker what kind of communication he will have with the patient. But in any case, the paramedic or nurse must follow certain tactics in relation to the patient and, most importantly, the health worker, as a person, must have certain characteristics in all respects in order to earn the patient's trust in himself. Indeed, without trust, a normal relationship between a health worker and a patient is impossible. Consequently, the personality of the paramedic, the style and methods of his work, the ability to influence and treat patients are an important element not only of the treatment process, but also psychological communication healthcare worker and patient.
Bibliography
1. Grando. A.A. Medical ethics and medical deontology. Kyiv, Leading publishing house "Vishcha school", 1982, 168 pages.
2. Matveev. V.F. Fundamentals of medical psychology, ethics and deontology. Moscow, "Medicine", 1989, 178 pages.
3. Shkurenko. YES. General and medical psychology. Rostov-on-Don, "Phoenix", 2002, 352 pages.
Hosted on Allbest.ru
Similar Documents
Communication and its importance in medical activity. Features of the relationship between the patient and the health worker. Nurse and patient - the principles of communication with the patient. Types of nurses and their characteristics. The role of the nurse in communicating with the patient.
abstract, added 05/14/2008
The essence and content of the concept of professionally significant qualities of the personality of a medical worker. Psychological requirements for personality nurse. results empirical research the success of the nursing staff.
term paper, added 02/15/2013
Aspects of problems of difficult communication. Factors that create difficulties in communication, the reasons for their occurrence. Psychological classification of communication types. General characteristics of personality and difficulty in communication. The influence of communication on personality, personality on communication.
term paper, added 01/31/2016
The essence, functions and types of communications, their role and significance in the workforce. The specifics and patterns of communication of employees in the organization. The study of self-disclosure of personality in interpersonal communication. Finding out the motives of self-disclosure in this process.
term paper, added 12/16/2015
The concept, types and functions of communication, characteristics and significance in the psychological development of a person. Technique and methods of communication. The main stages that the ontogenetic development of human communication goes through. Techniques for the study of values and meanings of personality.
term paper, added 05/23/2009
The concept of communication, its goals, objectives, functions, varieties. Psychological characteristics of the leader's personality. The specificity of thinking in the activities of the manager. Factors influencing the choice of the "key" of communicative communication. conditions for effective communication.
term paper, added 11/30/2014
Characteristics of the concept, functions, types of communication. Features of the formation of a person as a person, object and subject of communication. Styles of pedagogical communication and their technological characteristic. Mental features of communication in primary school age.
term paper, added 02/04/2010
abstract, added 11/13/2015
The role of communication in the mental development of a person. Aspects and types of communication. The structure of communication, its level and functions. The concept of encoding information in the process of communication. Interactive and perceptual aspects of communication. The accumulation of human culture of communication.
control work, added 11/09/2010
Study of the influence of the phenomenon of communication on the mental development of the individual, on the moral sphere, worldview. The concept of communication: types, functions, classification. Disclosure of the views and works of Vygotsky, Leonov, Gippenreiter on the role of communication in personality development.

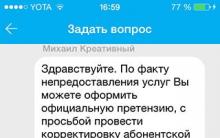
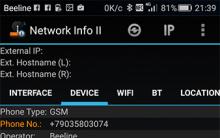







How to disable ads on Android: remove pop-up ads
The Russian received a term and a million fine for "piracy Negative consequences of the law
Identification of key factors
The criteria for classifying organizations and individual entrepreneurs as small and medium-sized businesses have changed
See what "Royalty" is in other dictionaries Pitfalls of legislation